Hearts 101: Common Heart Diseases
Information is power. If you understand your heart and the things that can go wrong, you will ask better questions and receive better care.
I've always been an educator, and I felt it was important for my patients to have a basic understanding of their heart anatomy before they could understand what was going wrong. These days, in our fast-paced world of medicine, there is little time to teach patients, so it's often left to you to do your own research. I hope that this series of education blogs gets that started. The extensive information used in researching this blog is itemized at the end under Sources and Resources.
Women have unique and often misunderstood issues. Please consider reading The Silent Threat of Women's Heart Disease.
One in two Canadians will be diagnosed with some form of cardiovascular disease in their lifetime.
Until the age of 65, men outnumber women two to one. After that, the protective effect of estrogen starts to wane, and women quickly catch up to men.
Cardiovascular disease includes hypertension, also known as high blood pressure, coronary artery disease, cardiomyopathy (enlargement of the heart muscle), peripheral vascular disease, and brain vascular disease. It accounts for 32% of deaths, which outranks cancer as the number one cause of death for those over the age of 75.
Atrial fibrillation is a disease of the electrical system, and while it can be driven by cardiovascular disease, it can be due to a completely separate cause.
Below we will cover:
The Plumbing: Diseases of the Arterial System
Coronary Artery Disease
Angina
Myocardial Infarction, known as a Heart Attack
Coronary Microvascular Disease
Spontaneous Coronary Artery Dissection (SCAD)
Broken Heart Syndrome
The Mechanical System: Diseases of the Cardiac Muscle and Valves
Cardiomyopathy and Heart Failure
Valve Disease
The Electrical System: Abnormal Heart Rhythms
Atrial Fibrillation (AFib)
Heart Block
Ventricular Tachycardia and Fibrillation
The Plumbing: Diseases of the Arterial System
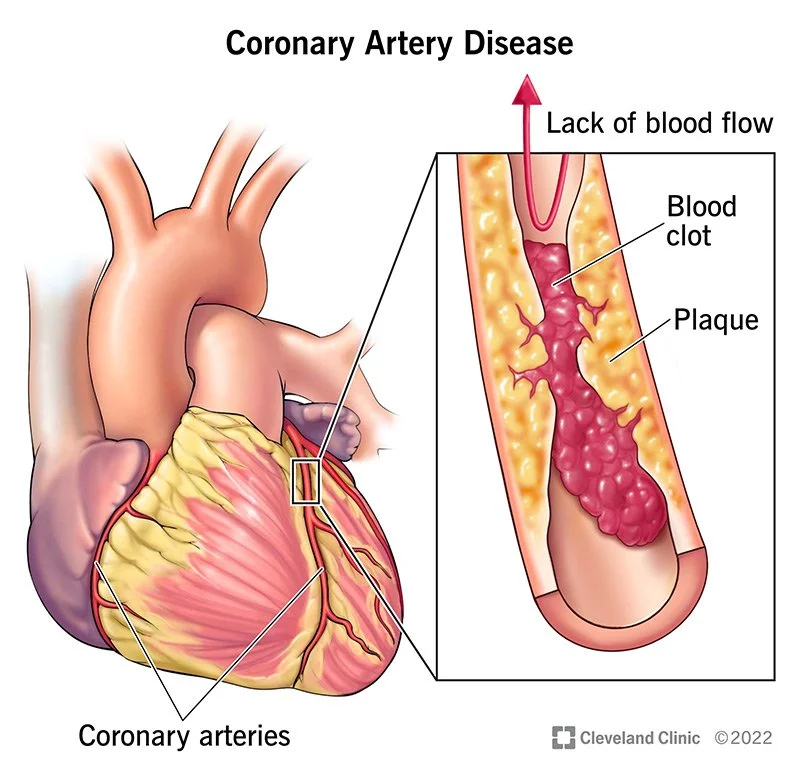
Coronary Artery Disease impacts the major vessels called coronary arteries, which run over the outmost layer of your heart. This unique organ biology means that the vessels are easy to see and repair with open-heart surgery. Fatty deposits and calcium build up inside the arteries, forming plaques that reduce or completely block blood flow. These deposits build up over our lifetime, and there are rarely any symptoms until the blockages are significant.
Risk factors for all types of cardiovascular disease are high blood pressure, diabetes, elevated cholesterol, obesity, smoking, a diet high in fat, saturated fats and processed foods, some forms of autoimmune disease (especially vasculitis) and rheumatological disorders, strong family history; a sedentary lifestyle.
Prevention and Interventions include lifestyle changes, including weight loss, prescribed exercise programs, and diabetes management; statin medications to lower cholesterol levels and prevent further blockages; anticoagulants (blood thinners) such as Aspirin to prevent heart attacks; and medications to open the arteries and those to increase the efficiency of the heart while decreasing its workload.
Angina is not a disease – it is a warning sign of coronary artery disease and a possible myocardial infarction. It is caused by narrowing – but not complete blockage – of the coronary arteries, causing decreased oxygenated blood to the heart muscle.
Common Signs and Symptoms include increased shortness of breath with previously easy activities, discomfort in the central chest, especially with stress or exercise, aching in the neck, jaw, or left or right arm, nausea, and indigestion, all of which ease or go away with rest. Serious symptoms include waking with any of these symptoms and/or when the symptoms do not ease with rest or nitroglycerine within 15 minutes.
When angina is unstable (is worsening or comes on at rest despite medication management), a heart catheterization with a stent* (a mesh device that holds the artery open) might be recommended.
*Please note that it is a stEnt (with an ‘e’) and not a stInt (with an ‘i’).
The number one symptom of a cardiac event is denial. It is better to risk feeling embarrassed than being dead.
Visualize a massive old oak tree and turn the image upside down.
Myocardial Infarction (MI), commonly known as a Heart Attack
Visualize a massive old oak tree and turn the image upside down. The trunk is thick, supporting all of the other massive branches. Then, there are the tiny branches that hold the leaves that reach for the sun and the rain, feeding the entire tree. If a branch is cut off, the tree will continue to live. But cut the tree at the base, and the tree will die.
The same is true for the coronary arteries: The trunk of the coronary arteries is a vessel coming off the massive Aorta. The branches of the trunk wind around the heart. The tiniest vessels are within the heart muscle, feeding it oxygen and removing waste and carbon dioxide.
Fat and calcium plaques are gradually deposited under the innermost layer of the coronary arteries over a lifetime. Sometimes, these plaques are hard and 'stable,' and sometimes, they are 'unstable' (soft and not compact). Unstable plaques are the primary cause of MIs. When an unstable plaque ruptures, the body's clot factors rush to the site, forming a clot and completely occluding (blocking) the artery. Immediately, all heart cells that rely on the oxygenated blood from that artery will begin to die.
If a blockage is in a distant branch, damage can be minimal, but the closer the blockage is to the trunk, the more damage will take place. If the blockage is in the main trunk – the Left Main – death is almost immediate and is called a 'widow maker.'
Classic Signs and Symptoms are central chest pain, tightness, or squeezing. Men, in particular, say that it feels like an elephant standing on their chest. Aching or pain can travel down the left arm (and sometimes the right), up the neck, and into the jaw. Sometimes, the only symptoms are the feeling of indigestion, nausea and vomiting. When I was a cardiac nurse, I would see patients become very still, very pale, and experience cold sweats; those patients would have me running to intervene.
Time is muscle! Call 911!
If the patient refuses to have you call, say they can go by car, or says they will drive themselves, this is another warning sign of denial. Ignore them. Call 911.
Interventions include immediately chewing two baby Aspirin to reduce and break up the clotting action. Once at the hospital, the gold standard of treatment is an immediate heart catheterization and a stent to open the affected vessel(s) or immediate open-heart surgery. If the adult is in a hospital that does not have a heart catheterization lab, major clot-busting medications should be given. If a stent has been inserted, medication management usually includes a blood-thinner (anticoagulant) and others to reduce the workload and increase the efficiency of the heart.
Surviving a heart attack should be the ultimate wake-up call to make lifestyle and dietary changes for the rest of one’s life.
Coronary Microvascular Disease affects the microvasculature – the small blood vessels that come off of the large blood vessels and penetrate and nourish the muscle tissues. This is now referred to as INOCA or Ischemia (inadequate blood flow) with Non-obstructive Coronary Arteries. Damage occurs to the inner walls of small vessels, resulting in microvascular angina and spasms disrupting blood flow. Small vessel disease is more likely to affect women than men. This is especially true during menopause, when estrogen levels begin to decrease.
Although the affected arteries may be small, the symptoms can have a big impact on a person's quality of life. Similar to those caused by obstructive coronary artery disease, the symptoms can include shortness of breath or trouble exercising. INOCA can also increase a person's risk of hospitalization for a heart attack, heart failure, and death. Harvard Medical School.
The most common symptom is central chest pain, heaviness, or tightness that does not subside with rest and lasts longer than 15 minutes.
The most accurate testing is done by PET scan.
Lifestyle changes, especially extremely good diabetic control, and medication changes to improve heart disease risk factors may be beneficial.
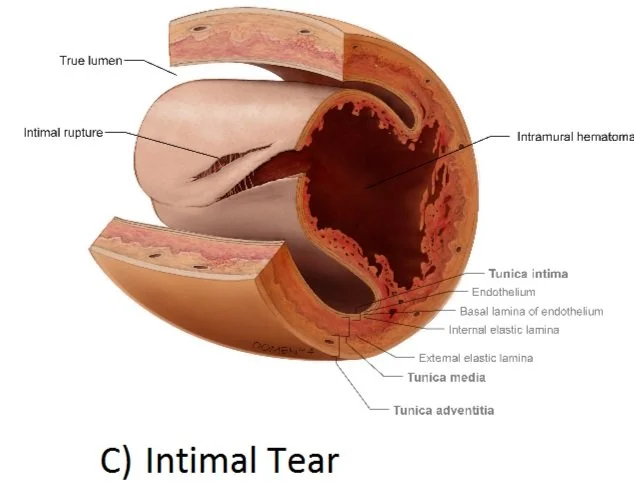
Spontaneous Coronary Artery Dissection (SCAD) is under-diagnosed and poorly understood. Over 90% of cases are in women, primarily those in or after menopause. It is the cause of myocardial infarction (MI) in 24% of women over the age of 50 but is frequently missed on coronary angiography.
SCAD is an emergency condition that occurs when a tear forms in a wall of a heart artery. It can slow or block blood flow to the heart, causing a heart attack, heart rhythm problems or sudden death. People who have SCAD often do not have risk factors for heart disease, such as high blood pressure, high cholesterol or diabetes.
Symptoms are the same as for myocardial infarction (MI), aka heart attack. Seek immediate emergency intervention for severe chest pain radiating down either arm or jaw, nausea and vomiting.
Broken Heart Syndrome (Takotsuko Syndrome)
80 to 90% of patients with broken heart syndrome are women.
Since the beginning of time, it has been said, "She died of a broken heart." Science didn't catch up with this phenomenon until 1990, after a major earthquake, when Japanese hospitals were inundated with people – mostly women – complaining of classic heart attack symptoms. Cardiologists performed heart catheterizations and saw bizarre changes in the grieving heart.
There were no blockages, no ECG changes, and blood markers that point to a heart attack were negative. However, as the heart was contracting, the top of the heart was contracting extremely vigorously, so much so that it blocked the outlet of the left ventricle, while the bottom of the heart was almost immobile. It produced a shape like a balloon or a narrow-necked pot. It reminded the Japanese doctors of the pots called Takotsubo that were used to trap octopuses. and thus, the syndrome got its new name.
With all other cardiovascular diseases, men outnumber women by more than two to one before the age of 65. But, 80 to 90% of patients with broken heart syndrome are women. An even more striking feature is that most of them recovered completely, with no sign of cardiac damage. They went from an emergency admission with severe chest pain and some with acute heart failure to walking out of the hospital disease-free, sometimes in a matter of days.
“It is a very sobering fact to think that women suffering from Takotsubo syndrome might have been dismissed as malingers before such an imaging was possible. You can see how a middle-aged woman, distraught after an upsetting event, coming into the hospital with chest pain and collapse but recovering quickly might have been seen as having had a hysterical illness. Taking this even further, many people who have had panic attacks say, ‘I thought I was having a heart attack, but I was fine after a while.’ Maybe they were Takotsubo sufferers too?” Sain E. Harding, The Exquisite Machine
The Mechanical System: the Cardiac Muscle and Valves
The Power of Relaxation: Heart failure is due to inefficient relaxation of the heart muscle due to ventricle muscles that are scarred, thickened, or floppy.
In order to understand heart failure, it's important to understand the incredible power of a healthy heart. Your heart pushes blood through 60,000 miles of blood vessels. The right ventricle has to push blood to the lungs. Then, with every heartbeat, the blood circulating in the lungs is pushed back to the heart. Then, the left side of your heart pushes oxygenated blood to your entire body.
The heart muscle needs to generate a strong and very rapid force. Then, it needs to rest in order to refill. The faster it can do this, the more effective the beat.
The Power of Relaxation: Heart failure is due to inefficient relaxation of the heart muscle due to ventricle muscles that are scarred, thickened, or floppy.
Heart function is measured by its Left (ventricle) Ejection Fraction (LEF): the percentage of blood the left ventricle is able to push out with each contraction. Normal LEF is 50 to 75%. Even an elite athlete's heart can't push 100% of the ventricle's blood.
Mildly reduced LEF is between 41 and 49%. A reduced LEF is 40% or less.
Some things that may cause a reduced ejection fraction are:
Weakness of the heart muscle, such as cardiomyopathy.
Heart attack that has damaged the heart muscle.
Heart valve disease.
Long-term, uncontrolled high blood pressure.
Cardiomyopathy and Heart Failure
Heart failure is not the same as a heart attack. A heart attack – or the ongoing damage, scar tissue, and inflammation from a heart attack can cause heart failure. When a heart attack causes it, it can be immediately life-threatening.
Other causes are long-term damage from pollution, noise, stress, uncontrolled blood sugars, damage from smoking, drug and chemotherapy toxicity, and inflammatory responses to bacteria, viruses, and COVID. Heart failure is the primary reason patients are monitored in a critical care unit.
Cardiomyopathy is a disease of the heart muscle that causes heart failure. Within the heart muscle, heart cells called cardiomyocytes are replaced by scar tissue that is neither electrically conductive nor contractile. There are at least eight different sub-categories of cardiomyopathy. There is no cure, and nothing can be given to reverse the condition, but symptoms and further damage can often be effectively treated.
The words 'heart failure' are scary. It is a condition that needs to be dealt with and treated with all due seriousness and speed to save heart tissue and maintain quality of life. Some people die after one acute and sudden event of heart failure, but others live many years in what is a manageable chronic condition. It is always progressive but can most often be well managed with lifestyle changes and medications.
Common Signs and Symptoms of chronic heart failure can come on slowly, and people often adapt without realizing something is wrong. Left-sided heart failure symptoms most commonly include chronic breathlessness, fatigue, and swelling of the feet, ankles, and lower legs. Symptoms of right-sided heart failure include fluid retention in the abdomen, difficulty breathing when lying flat, dizziness, and fatigue.
Serious, life-threatening symptoms are severe shortness of breath, a wet cough with clear, frothy, blood-tinged sputum, and an erratic heart rhythm.
Interventions include oversight by a cardiologist or, better yet, a heart function clinic. Often, several medications are needed. A prescribed and monitored exercise program is key, and diet management is vital.
Valve Disease
Hearts have four valves. They have two (bicuspid) or three (tricuspid) leaflets. Each valve carries varying pressure loads. They open as the atrium or ventricle pushes blood flow into the next chamber, and they close at the end of the beat. They prevent the backflow of blood into the chamber the blood has just left from the previous chamber. Each valve will have opened and closed as many as 3 billion times if you reach the age of 80. See A Love Letter to Your Heart.
Most people have no idea they have valve disease unless a doctor picks up the abnormal sounds – a murmur – while listening to your heart, or valve disease is so advanced that symptoms cause significant interference with daily tasks.
The most common issue is stenosis (narrowing), which occurs when the leaflets harden and can no longer open and close properly. Valve wear can also occur with age. The aortic and mitral valves are most often affected.
If a bacterial infection is present in the bloodstream, it may infect the innermost lining of the heart and its valves, causing endocarditis. This condition must be treated emergently with prolonged courses of strong antibiotics and, sometimes, surgical replacement of the valves. If not treated promptly and aggressively, this condition is often fatal.
The most common symptom of any valve issue is shortness of breath. If the heart is under ongoing strain, heart failure will also occur (see above).
Interventions include medications to reduce the heart's workload, prescribed exercise programs, and ongoing monitoring of valve status. The only definitive cure is surgical replacement of the affected valves.
The Electrical System: Natural Pacemaker and Conduction Nerves
It's important to understand the electrical pathways of the heart. Please review A Love Letter to Your Heart.
Atrial Fibrillation (AF) = AFib
The most common electrical condition of the heart is Atrial Fibrillation. In this condition, the top chambers—the atria—no longer respond to the SA Node's (natural pacemaker) signals and beat chaotically on their own. Many people do not experience symptoms, but others feel a sensation of butterflies in their chest.
In ‘Uncontrolled AFib,' the atrium can beat more than 130 beats per minute. When the atrium beats erratically, so do the ventricles, resulting in an irregular pulse. At that point, the adult may feel weak, dizzy, short of breath, and even faint (syncope). An episode of uncontrolled AFib is often the first time that a person seeks medical attention.
AFib is the number one cause of brain strokes. When the atria do not beat efficiently, blood clots can form. Think of a tidal pool eddy where the water swirls and is not taken out to the main water. With a strong contraction, pieces of the clot break off and are sent to the lung, to the heart muscle itself, but most commonly to the brain, causing a blockage in a brain artery.
Interventions: Patients with atrial fibrillation are automatically put on anticoagulants for the rest of their lives, even if their heart has returned to a normal rhythm. Once AFib has occurred, the chances of it coming back, becoming more frequent or even permanent, are high. Additional medications help the heart stay in a regular rhythm and beat more efficiently.
Catheter Ablation: If AFib rates are often above 100 beats per minute, and the patient is often symptomatic (short of breath and weakness), a catheter 'ablation’ might be recommended. The BC Centre of Excellence is St. Paul’s Hospital:
“An electrode on the end of a catheter is threaded to the heart, where it produces heat (or cold) to create tiny scars in targeted areas of heart tissue. This interrupts the arrhythmia and restores the heart's normal rhythm. Often, the procedure needs to be repeated.” St. Paul’s Hospital
Heart Block, also known as Bundle Branch Block
Heart block occurs when heart damage affects the electrical signal flow between the atrium and the ventricles via the central wall. The only symptom might be a slow heart rate. Heart block is usually discovered on an ECG and rated first, second, or third-degree. First- and second-degree heart block are generally untreated, but third-degree heart block must be treated with the insertion of a pacemaker.
Ventricular Arrhythmia: Tachycardia (VT) or Ventricular Fibrillation (VFib)
These are extremely rare electrical events that cause cardiac arrest and death unless CPR and defibrillation (use of an AED*) are immediate. A large heart attack most often causes it, or it can be from structural changes to the heart, such as cardiomyopathy. Other causes are drug overdoses, a large electrical shock, blunt-force trauma to the central chest (examples include a car accident when the airbag didn’t deploy or a sports hit to the chest), and genetic predispositions.
The ventricle no longer contracts in a coordinated way, and different areas contract and relax at different times and speeds, so it wriggles and turns without ejecting blood. Surgeons who see this during an operation when the chest is open describe it as looking like a bag of worms.
Interventions: People at high risk of sudden ventricular arrhythmia may have an internal defibrillator inserted in their chest and attached to their heart. This large pacemaker detects abnormal rhythms and delivers an electrical jolt to restore the heart to a normal rhythm.
*I have inserted a link for a home AED at the end of Sources and Resources (Thanks, Marjie)
We Can Help
If you've been diagnosed with a heart condition, please reach out to learn how we can work together to ensure you receive timely care. As a former cardiac nurse and seasoned patient advocate, I've seen firsthand how easily patients can fall through the cracks, their referrals misplaced and appointments delayed. I specialize in helping BC residents navigate our cardiac healthcare system, and my support can help save precious months - maybe even your life. Let’s chat.❤️
Sources and Resources
Angina Treatments: National Institute for Health (NIH)
Aortic Calcification: Mayo Clinic
Atrial Fibrillation: Canada Heart & Stroke
Blood Vessels: Cleveland Clinic
Cardiomyopathy: BC Heart & Stroke
Cardiomyopathy: Mayo Clinic
Cardiomyopathy Types: NIH
Coronary Artery Disease: Cleveland Clinic
Coronary Calcium Scan: Mayo Clinic.
Coronary Microvascular Disease: Cleveland Clinic
Coronary Microvascular Disease: Harvard School of Medicine
Endocarditis: Cleveland Clinic
Heart Failure: Diagnosis and Treatment: Government of BC
Heart Failure Symptoms: HealthLink BC
Heart Valve Disease: Mayo Clinic
Spontaneous Coronary Artery Dissection: Mayo Clinic
Takotsubo Cardiomyopathy POD: Maimonides Emergency Medicine
Ventricular Arrhythmia: Cleveland Clinic
The Exquisite Machine: Sean E. Harding
Home Use AED: HeartSine Samaritan AED 350P (reduced price for Costco members)